Gingival Disease Causes

Poor Oral Hygiene is a Major Cause of Gingivitis1
Take a closer look at the causes and mechanisms behind the condition, with a particular focus on why poor oral hygiene is the major cause of gingivitis1,2
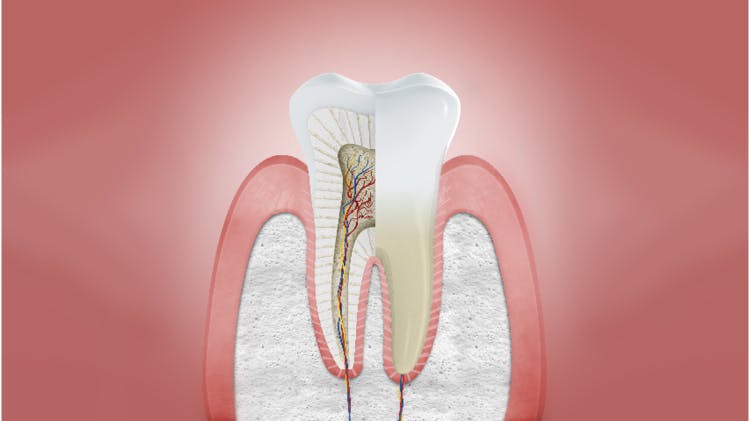
Gingivitis is Caused by Plaque2
- The number one cause of gingivitis is due to the buildup of plaque and bacteria along the gingival margin and between the teeth2
- Endotoxins and bacterial debris released by these plaque bacteria cause inflammation in the surrounding gingivae known as gingivitis1,2
- If plaque is not removed, over time this inflammatory response can become chronic, leading to progressive tissue and bone destruction1

Patients may ignore or not to be aware of the signs of poor gingival health
The early symptoms of gingival disease may be ignored for a number of possible reasons:3
- Lack of awareness of gingival health importance (believing bleeding gingivae to be ‘normal’)
- A belief that teeth are more important than gingivae
- More focus on current cosmetic issues, rather than on possible future issues caused by periodontal disease
- Expect dental practitioner to fix gingival issues instead of proactively managing own gingival health
Progression Of Gingival Disease
Gingivitis is a reversible condition that develops when plaque builds up around the gingival line which induces inflammation of the gingivae. If left untreated, chronic gingival inflammation can progress into chronic periodontitis, causing bone loss and potential tooth loss.1,2
Healthy gingivae
Uninflamed gingivae without any of the signs of periodontal disease. Characteristics include:4
- Pale pink and firm gingivae
- Stippled
- Firmly attached to teeth
- Knife-edge margin
- Not normally prone to bleeding on brushing or probing

Gingivitis
Reversible plaque-induced inflammation of the gingivae.1Characteristics include:4
- Change in color of the gingivae
- Marginal gingival swelling and blunting of the gingival papillae
- Bleeding on probing and brushing
- Probing depth of gingival crevice does not exceed 3mm
- Gingival attachment remains unchanged, no bone loss
Bleeding on probing should be the primary signal to identify gingivitis.4 If a patient has gingivitis this can be reversed with a gum health regimen, but a periodontitis patient remains a periodontitis patient for life, even following successful therapy, and requires life-long supportive care to prevent recurrence of disease.5 This is one of the reasons it is so important to manage the disease before it becomes chronic.5
A New Classification Of Periodontitis
In 2017 the American Academy of Periodontology (AAP) and the European Federation of Periodontology (EFP) along with expert participants from all over the world held a World Workshop to revise the periodontal classifications. The group was charged with updating the 1999 classification of periodontal diseases and conditions and developing a similar scheme for peri-implant diseases and conditions.5 The forms of the disease previously recognized as "chronic" or "aggressive", now grouped under a single category, "periodontitis".6
Periodontal Health, Gingival Diseases/Conditions5
Periodontal health & gingival health |
|
Gingivitis- dental biofilm induced |
|
Gingival diseases – non-dental biofilm induced* |
|
Forms of Periodontitis
Necrotizing periodontal diseases |
|
Periodontitis as a manifestation of systemic diseases |
Classified according to the International Statistical Classification of Diseases and Related Health Problems (ICD) codes |
Periodontitis |
|
Table adapted from Caton G et al. J Periodontol 2018; 89(suppl 1): S1-S84
*Parodontax has been studied in patients with plaque induced gingivitis.

Forms of Periodontitis
Periodontitis (under the new classification):5
Stage I: Initial Periodontitis
Stage II: Moderate Periodontitis
Stage III: Severe Periodontitis with potential for additional tooth loss
Stage IV: Severe Periodontitis with potential for loss of the dentition
Staging and Grading Periodontitis7
Periodontitis: staging
Staging is designed to classify the severity and extent of a patient’s disease based on the measurable amount of destroyed and/or damaged tissue as a result of periodontitis and to assess the specific factors that may play a role in the complexity of long-term case management.
Initial stage should be determined by clinical attachment loss (CAL). If CAL is not available radiographic bone loss (RBL) should be used. Tooth loss due to periodontitis may modify stage definition. Complexity factors may shift the stage to a higher level.
| Periodontitis | Stage 1 | Stage 2 | Stage 3 | Stage 4 | |
| Serevity | Interdential CAL | 1-2 mm | 3-4 mm | 5mm | 5mm |
| RBL | Coronal third (<15%) | Coronal third (15% - 33%) | Extending to middle third of root and beyond | Extending to middle third of root and beyond | |
| Tooth loss (due to periodontitis) | No tooth loss | <4 tooth | <5 tooth | ||
| Complexity | Local |
|
|
In addition to Stage 2 complexity:
|
In addition to Stage 3 complexity: Need for complex rehabillitation due to:
|
| Extent and distribution | Add to stage as description | For each stage, describe extent as:
|
|||
Periodontitis: grading7
Grading aims to indicate the rate of progression of periodontitis, responsiveness to standard therapy and potential impact on systemic health.
Clinicians should initially assume grade B disease and seek specific evidence to shift to grade A or grade C.
| Progression | Grade A: slow rate | Grade B: moderate rate | Grade C: Rapid rate | ||
Primary criteria Whenever available, direct evidence should be used. |
Direct evidence of progression | Radiographic bone loss or CAL | No loss over 5 years | <2 mm over 5 years | >2 mm over 5 years |
| Indirect evidence of progression | % bone loss / age | <0.25 | 0.25 to 1.0 | >1.0 | |
| Case phenotype | Heavy biofilm deposits with low levels of destruction | Destruction commernsurate with biofilm deposits | Destruction exceeds expectations given biofilm deposits; specific clinical patterns suggestive of periods of rapid progression and/or early onset disease | ||
| Grade modifiers | Risk factors | Smoking | Non-smoker | <10 cigarettes/day |
>10 cigarettes/day |
| Diabetes | Normoglycemic/no diagnosis of diabetes | HbA1c <7.0% in patients with diabetes | HbA1c >7.0% in patients with diabetes | ||
Three steps to staging and grading a patient
Step 1: Initial Case Overview to Assess Disease7
Screen
- Full mouth probing depths
- Full mouth radiographs
- Missing teeth
- Mild to moderate periodontitis will typically be either Stage I or Stage II
- Severe to very severe periodontitis will typically be either Stage III or Stage IV
Step 2: Establish Stage7
For mild to moderate periodontitis (typically stage I or II):
- Confirm clinical attachment loss (CAL)
- Rule out non-periodontitis causes of CAL (e.g. cervical restorations or caries, root fractures, CAL due to traumatic causes)
- Determine maximum CAL or radiographic bone loss (RBL)
- Confirm RBL patters
For moderate to severe periodontitis (typically stage III or IV)
- Determine CAL or RBL
- Confirm RBL patterns
- Assess tooth loss due to periodontitis
- Evaluate case complexity factors (e.g. severe CAL frequency, surgical challenges)
Step 3: Establish Grade7
- Calculate RBL (% of root length x 100) divided by age
- Assess risk factors (e.g. smoking, diabetes)
- Measure response to scaling and root planing and plaque control
- Assess expected rate of bone loss
- Conduct detailed risk assessment
- Account for medical and systemic inflammatory considerations
For further information on the 2017 World Workshop on the Classifications of Periodontal and Peri-Implant Diseases and Conditions visit perio.org/2017wwdc
Other Periodontal Conditions
Risk Factors for Periodontal Disease can be Divided into Two Categories4
Modifiable Risk Factors
Local4,9
- Plaque and calculus
- Deficient dentition including open contacts, and overhanging and poorly contoured restorations
- Anatomical factors including malpositioned teeth, furcations, root grooves and concavities, and enamel pearls
Systemic4,9
- Poor oral hygiene
- Smoking and tobacco
- Stress
- Poor nutrition
- Diabetes mellitus (poorly controlled)
- Taking medications that cause xerostomia or that may induce gingival enlargement or pseudo-pocketing
Targeting modifiable risk factors, such as poor oral hygiene, can improve gum health management and treatment outcomes
Non-Modifiable Risk Factors4,9
- Family history and genetic factors
- Some hormonal variations, e.g. puberty, pregnancy and menopause
- Underlying immunodeficiency
Help Your Patients on Their Journey to Healthy Gums
Impact on Patient Quality of Life
Find out about the impact periodontal disease has on patients’ daily lives.



