Designing Dentures

The Importance of Denture Design
A well-designed denture can restore chewing ability, improve speech, have aesthetic appeal and help maintain overall oral health.1
Creating functional and comfortable dentures requires careful custom planning and consideration of the following factors:1,2
- Clinical
- Anatomical
- Technical
Principles of Good Denture Design
Three overarching principles form the foundation of good denture design
- Retention: The denture should be resistant to the forces that can cause it to move away from supporting tissues.2,3
- Stability: The denture should be as stable as possible, resisting any lateral movement and avoiding constant reminders of its physical presence in the patient’s mouth.3,4
- Support: The denture should be resistant to the forces that may cause it to move.4

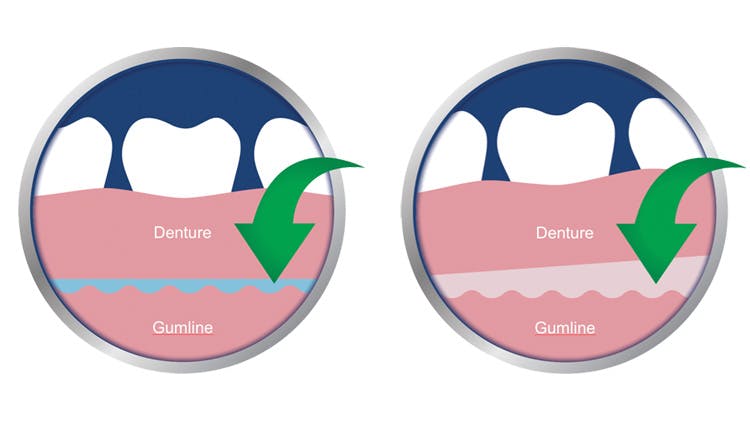
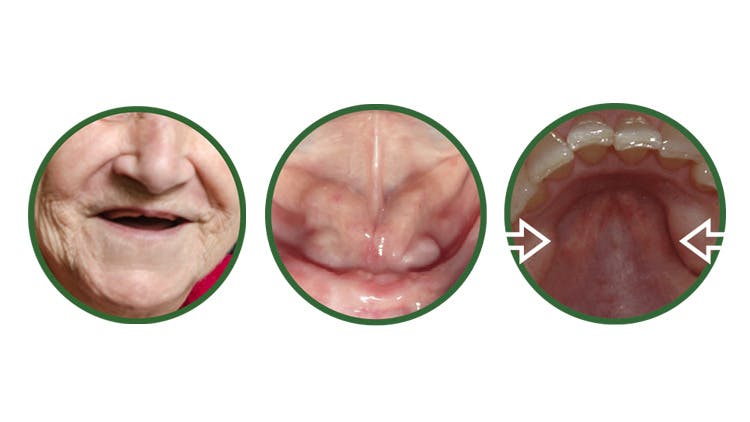
Restricted oral anatomy and denture retention/stability
Restrictions in patient oral anatomy can limit denture retention and stability.4,5Well-fitting denture performance can be limited by patients’ oral anatomy,6 and can be gradually affected by bone resorption over time.6,7
Impact of oral anatomy
Factors limiting retention:
- Surface area defined by individual oral anatomy
- Gradual physiological bone resorption over time6,7
Patient impact:
- Low denture retention and stability6,7
- Poor chewing ability6
- Poor denture satisfaction7
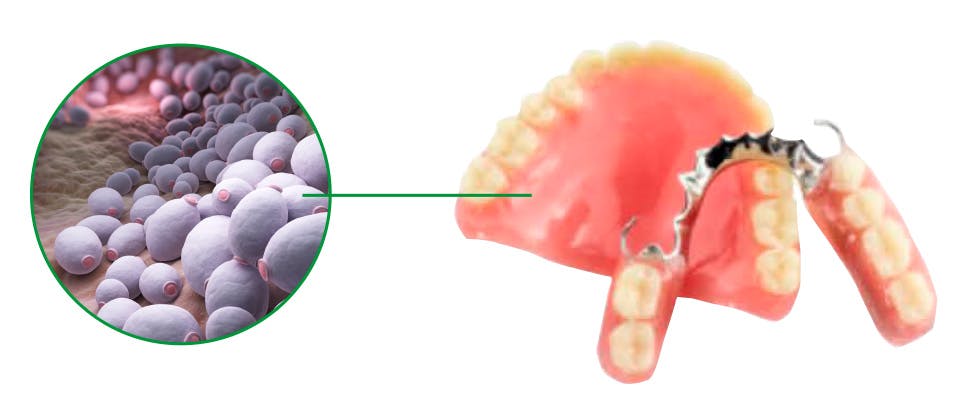
Poor Denture Hygiene Can Compromise Oral Health8
Inadequate Denture Cleaning May Lead to Denture Stomatitis12,13

Up to 88% of denture wearers do not clean their dentures effectively.14

Up to 67% of full denture wearers have denture stomatitis.12

Denture stomatitis
Denture stomatitis is commonly associated with a yeast infection that causes the area underneath the denture to become very red.
Left untreated, it causes soreness of the mouth and may lead to poorly fitted dentures in the future.12,13
Stomatitis* is caused by microbial biofilm on the denture-fitting surface (rather than the mucosal surface) and poorly fitted dentures.13
The prevalence of denture stomatitis is strongly linked with the amount of denture plaque.12
*Polident not indicated for treatment of denture stomatitis
Effective education can reduce the risk of inadequate dental hygiene practices
Medical conditions and hygiene proficiency affect denture performance

Patient Implications of Xerostomia
Reduced retention of dentures caused by xerostomia predisposes patients to mucosal abrasions and ulcerations.4
Help Your Patients on Their Journey to Optimal Denture Care
Impact on Patient Quality of Life
Find out about the impact that dentures have on patients’ daily lives.
Oral Health Management
Explore an overview of diagnozing issues with denture performance.