Allergic Rhinitis Causes & Mechanisms

Allergic cascade—what happens when an allergen infiltrates the body?
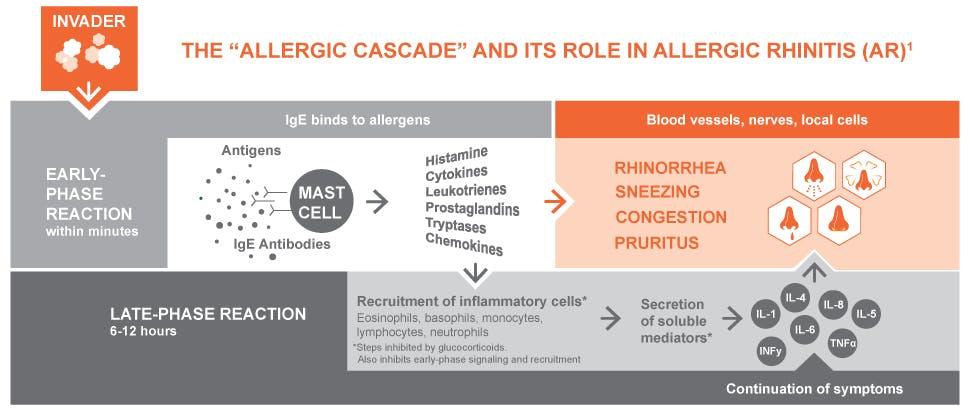
The “allergic cascade” and its role in allergic rhinitis (AR)1
The body’s immune response to allergens includes a series of early- and late-phase reactions—the allergic cascade. There are several allergic mediators involved in this cascade, not just histamines.2
Typically, the allergic cascade follows this pattern2,3:
- Sensitization to an allergen
- Early-phase response upon re-exposure to an allergen
- Late-phase response
When the body is exposed to an allergen:
- Sensitization involves being exposed to an allergen for the first time2
- The body produces immunoglobulin E (IgE) designed specifically for that particular allergen, but an allergic reaction does not yet occur2
- Re-exposure to an allergen triggers an early-phase response that occurs within minutes to an hour2
- The IgE of mast cells binds to the allergen, crosslinking the IgE2
- When enough crosslinking occurs, the mast cells explode with histamine and other inflammatory substances, called mediators, such as cytokines, leukotrienes, prostaglandins, eosinophils, and thromboxanes2,3
- The late-phase response occurs from 3 to 10 hours after allergen re-exposure2
- Immune cells, such as eosinophils, secrete substances that increase inflammation and bring other immune cells into the reaction, perpetuating the inflammatory response2
- Symptoms can be more severe than those in the early phase2
The end result is the allergic response consisting of a range of symptoms such as rhinorrhea (runny nose), sneezing, congestion, and pruritus (itching)2
Read more about allergic rhinitis



Impact on Patient Quality of Life
Find out about the impact allergic rhinitis has on patients’ daily lives\



The FLONASE family
Find out how our products can help your patients suffering from allergic rhinitis