Their pain is never just one word
Opening Pandora’s Box
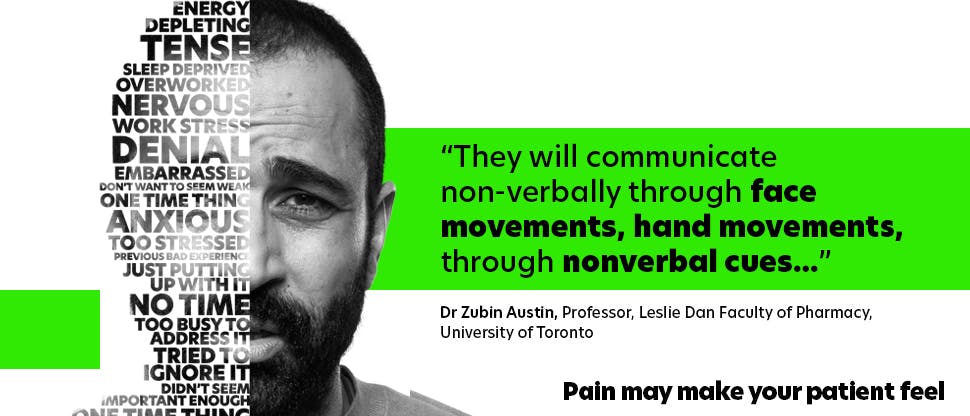
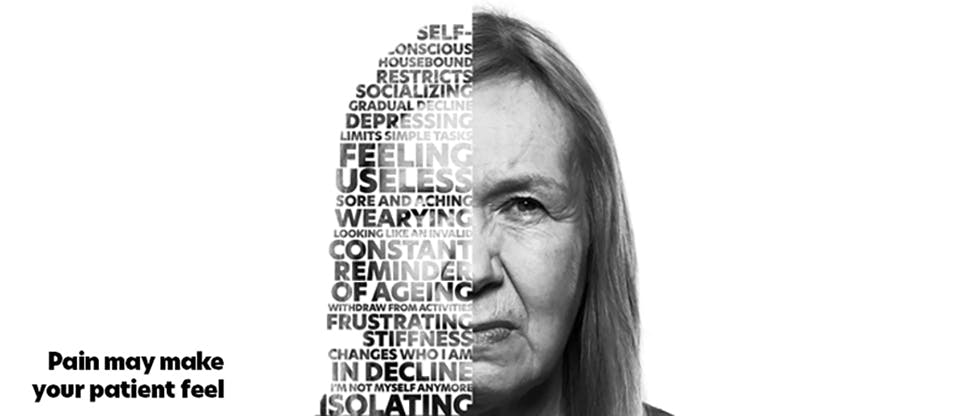
Asking patients about their pain experience can sometimes feel like opening Pandora’s Box. Unless you ask the right questions, it can be incredibly difficult to get the full context regarding someone’s pain. Even when they do open up, they might not give the full story, or they might go on and on. So, with limited consultation time, how can a health care professional (HCP) best explore a patient’s pain experience, to bring each individual sufferer the most appropriate, individualized pain management strategy? How can you maximize your time with your patients?
Better conversations for better clinical outcomes in pain management

A helping hand from Haleon
At Haleon, we believe in making sure that every patient gets the optimal outcome they need to manage their unique pain experience. The #ListenToPain campaign aims to equip HCPs with the knowledge and tools to better understand their patients’ pain.
We’re committed to providing HCPs with new tools and techniques, sharing the latest advances and bringing innovation that will allow you to better #ListenToPain.
Discover more pain management resources below
Products
Find out how our treatments can help your patients manage their acute pain and/or fever.
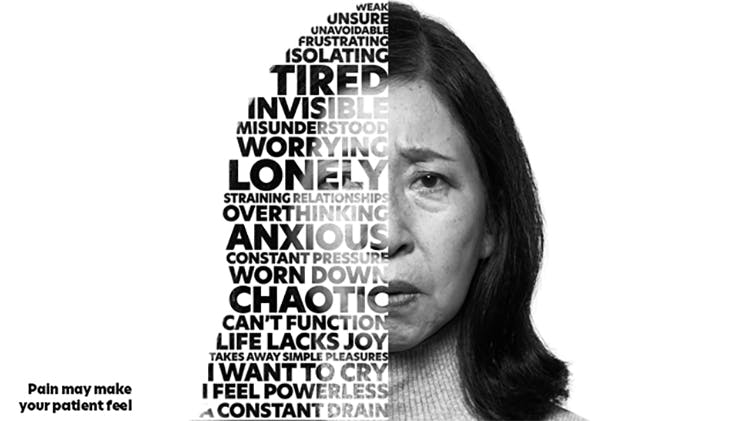
#ListenToPain
Discover a personalized approach to pain management. Better conversations for better clinical outcomes.
Patient care resources for personalized pain management
Access resources to facilitate better conversation around personalized pain management.