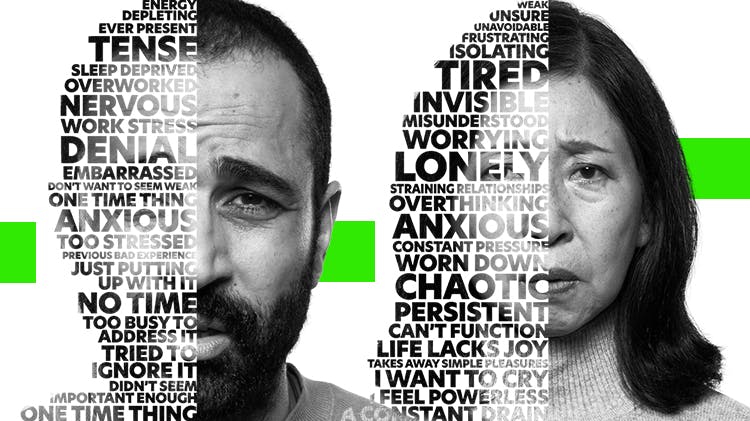
Their pain is never just one word
Opening Pandora’s Box
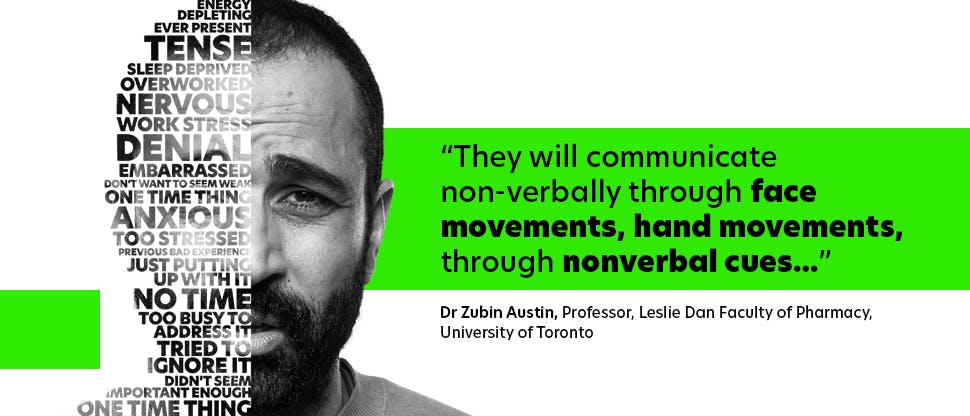
Asking patients about their pain experience can sometimes feel like opening Pandora’s Box. Unless you ask the right questions, it can be incredibly difficult to get the full context regarding someone’s pain. Even when they do open up, they might not give the full story, or they might go on and on. So, with limited consultation time, how can a health care professional (HCP) best explore a patient’s pain experience, to bring each individual sufferer the most appropriate, individualised pain management strategy? How can you maximise your time with your patients?
Better conversations for better clinical outcomes in pain management

A helping hand from Haleon
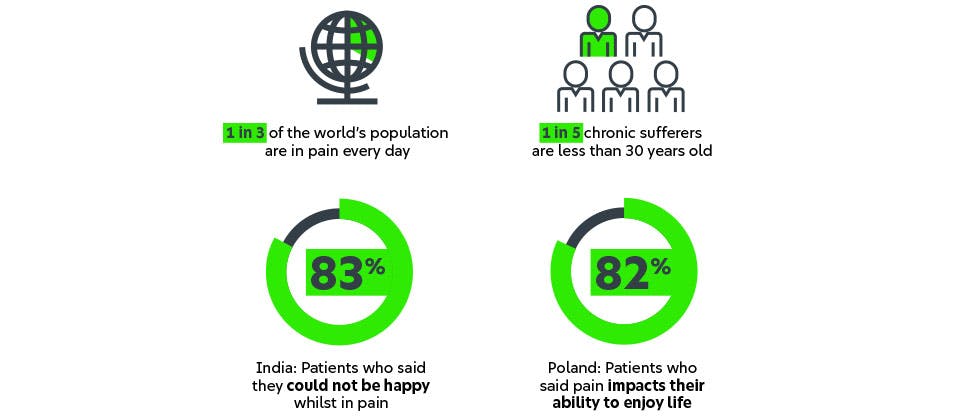
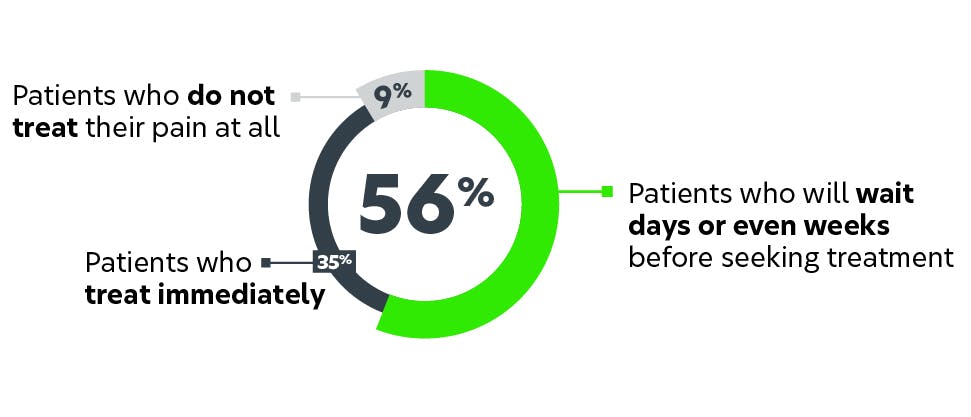
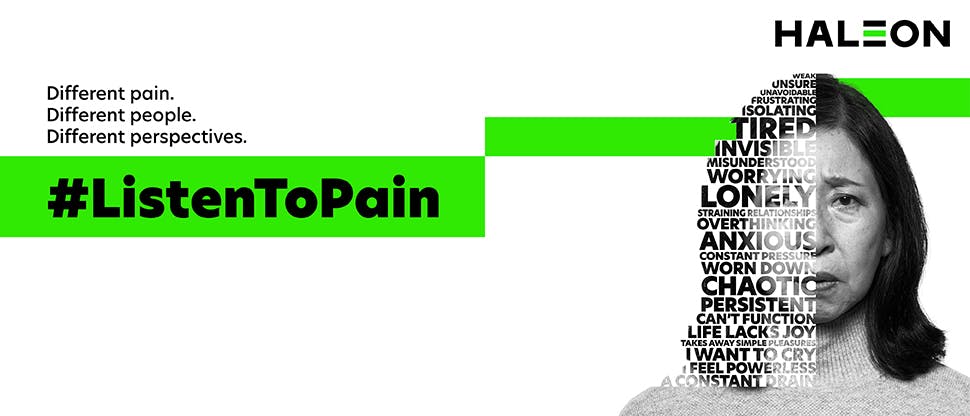
At Haleon, we believe in making sure that every patient gets the optimal outcome they need to manage their unique pain experience. The #ListenToPain campaign aims to equip HCPs with the knowledge and tools to better understand their patients’ pain. Using information from the Global Pain Index, we’ve established five different patient profiles, describing their relationship with and the handling of their pain. Based on a deep understanding of the human pain experience, these five profiles can help you maximise those precious minutes with patients and individualise your approach.
We’re committed to providing HCPs with new tools and techniques, sharing the latest advances and bringing innovation that will allow you to better #ListenToPain.
Discover more pain management resources below

Listen to Pain Webinars
Meet the experts who discuss about better ways to manage pain in everyday life.
#ListenToPain
Discover a personalised approach to pain management. Better conversations for better clinical outcomes.
Patient care resources
Access resources to facilitate better conversation around personalised pain management.