Tooth loss - a pivot point for future oral care

First Tooth Loss in Adult Patients
First tooth loss exerts a significant psychological impact on adult patients but can also be a pivotal point in protecting future oral health, with the added potential of strengthening patient-clinician relations. By adopting a patient-centred approach, dental practitioners can demonstrate empathy and understanding as patients undergo a physical and psychological transition to partial prostheses
Tooth Loss Causes & Management
There are multiple reasons why a patient has no other choice but to lose a tooth or teeth. It can be a sudden, traumatic loss for some, due to an accident or sports injury, or the final step with no chance of stabilising deterioration . Most commonly, it is due to caries and/or periodontal disease.
How patients experience this psychologically will also differ markedly, says Dr Koula Asimakopoulou, a Reader in Health Psychology, School of Dentistry, King’s College London. Dependent on the circumstances of their tooth loss, she adds: “Patients will be in different psychological stages, given how they have lost their tooth.”
Whatever the reason, tooth loss presents the dental practitioner with an opportunity, she believes, to change patient behaviours. “Research suggests that people go through those teachable moments at a time where some big health event comes and hits them, so a tooth coming out, it's an opportune moment for the healthcare professional to intervene,” says Dr Asimakopoulou.
Dental practitioners can utilise their understanding of patients’ psychological needs to enable them to both optimise their partial appliance use and assist them in retaining their remaining dentition via long-term behaviour change. A positive dental experience at this critical time for patients can lay the foundation for a relationship built on trust and support.
The Potential for Partial Dentures
Although improved oral health has reduced the number of edentulous patients requiring full dentures, there are now an estimated 650 million people globally wearing partial prostheses1
Despite its growing prevalence, the move to wearing a partial prosthesis is a life-changing event. A recent review found a significant number of patients struggled in accepting their tooth loss, felt less confident and were emotionally distressed, with a marked impact on social interactions and functional activities.2
Dr Samantha Rawdin, a New York-based prosthodontist knows first-hand the psychological toll tooth loss has on her patients. “It's a hard thing. It's an emotional thing, especially when it's a front tooth - that tends to be very, very hard for patients. There's a lot of shame that comes with it.”
Being non-judgmental is critical. She uses tooth loss as an opportunity to create a teachable moment: “It comes from a place of educating the patient and explaining: ‘Okay, this is why you lost the teeth, this is what we're going to do to replace those teeth and this is how we're going to maintain everything that you still have, so I don't want you to feel badly about this.’”
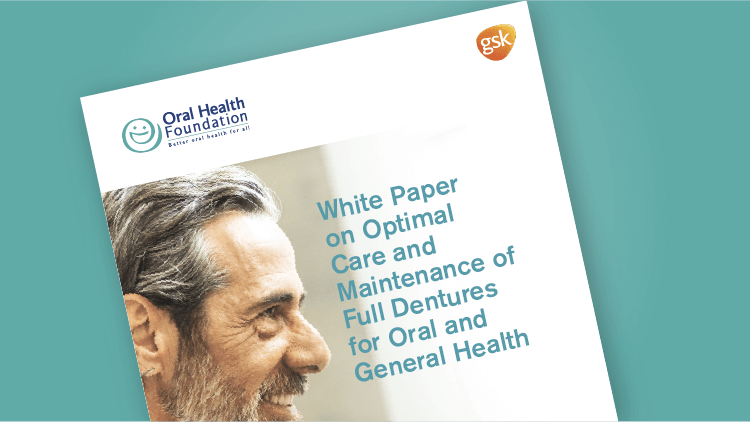
Recognising that patients may also be in different psychological stages of dealing with loss can help too, says Dr Asimakopoulou. “For example, in the situation of trauma, they were perfectly healthy, they have been doing all the right things all the time. And now they have lost a tooth. So, depending on where the person is within that cycle of grief when they come to see the dentist, there may be more or fewer opportunities to engage.”
The big change, says Professor David Felton, Dean and Professor at the School of Dentistry, University of Mississippi Medical Center, is the patient’s need to maintain the partial but also their remaining dentition. “There's an old adage in dentistry: You don't need to brush and floss all of your teeth, just the ones you want to keep.”
Learn more about the impact on quality of life
Figure 1: The cycle of grief (adapted from Kubler-Ross 1969)3
Making the Change to Partials – Motivating Patients
Making the transition to partials is a significant stage in patients’ psychological process where dental practitioner intervention is critical. Data show moving to partials provides benefits not only in appearance, but in overall oral health quality of life, improved social interactions and enhanced self-esteem and psychological well-being.4 However, this takes time.
“The big thing here, I think, is not only educating them, but to have them be patient,” adds Professor Felton. Patients need to recognise that having a new partial will not instantly return to them to their previous full dentition state, he explains: “For most people it takes quite a while, it can take a month or longer for them to adapt to it.”
Dental practitioner intervention is critical
Life with Dentures – Maintaining an Oral Hygiene Routine
Moscow and Volgograd-based prosthodontist Dr Petr Brinkovskiy says this adjustment can be dependent on patient motivation. “Some patients have a good motivation when they first start to use their prostheses. Some patients still have problems at one month, maybe two months. We sometimes need to meet maybe two, maybe three, maybe four times.”
He recommends taking before and after videos for patients to demonstrate the change in appearance. “Sometimes patients can’t smile, they can't eat and just after one week their life has changed because they have a beautiful smile. They see the picture before and after and it’s a good motivation.”
Dental practitioners may find that patients who already maintain a good oral hygiene regime could make an easier transition to partials and their care. “They understand what a regular oral care routine entails. Patients who are maybe just coming because they haven't been to a dentist in several years, I find that those are the patients that are harder to convert to a regular oral care routine,” adds Dr Rawdin.
Partials: The Patient Perspective
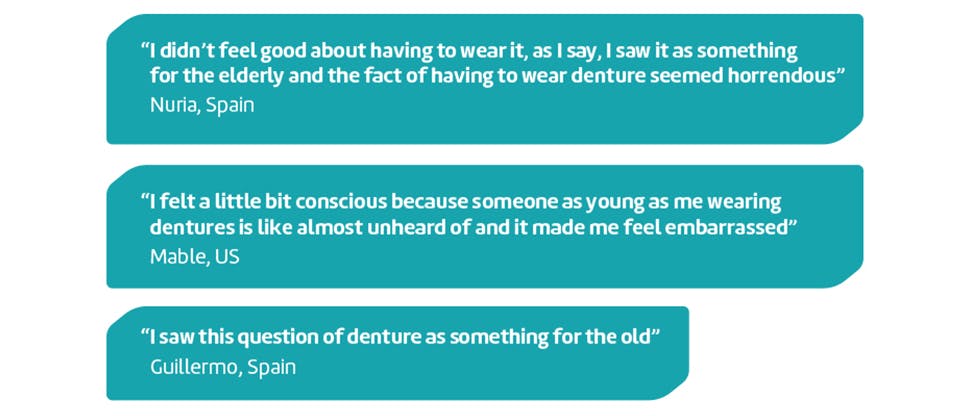
Interviews with patients in Russia, Spain and the US reveals the psychological impact of transitioning to partials, which can have an impact on transitioning to a new oral care routine at home.
Understanding Denture Care
Having patients understand that wearing partials means they have to change their oral health behaviour is “a critical part of the whole therapeutic goal”, says Professor Felton.
Dr Rawdin adds that it is important patients retain their remaining teeth as “without those, the partial may not function properly”.
Embedding a new oral care habit can be, as with other habitual behaviour, an idiosyncratic process, dependent on personally relevant behaviours.5 A patient’s previous oral care routine does not preclude them from changing once they have a partial as their behaviour can become a habit in one setting, but not in another.5 Data show that adopting a new habit consistently made it more likely to become automatic, but the time this took varied between 18 and 254 days, so patience with patients is required.6
For patients with partials, embedding a regular cleansing routine is essential. “A partial that stays in somebody's mouth for 8 or 10 or 12 or 15 hours a day, essentially underneath [the partial], it functions like a greenhouse to grow bacteria and oral biofilm,” explains Professor Felton. “Those types of things may not do a lot of damage to the partial, but it can do dramatic damage to the remaining teeth and soft tissues.” Indeed, a 10-year follow-up of patients with partials showed 20.5% of remaining teeth had been extracted, of which 66% were abutment teeth.7
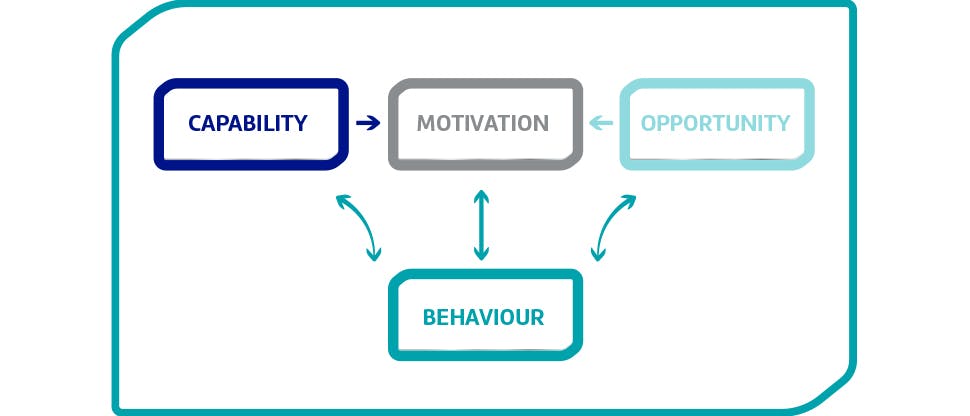
Figure 2: COM-B module of behaviour change (adapted from Michie, et al, 2011)8
Disrupting & Changing Behaviours
This period of transition to a life with a new partial could, however, offer a window of opportunity in changing the patient-professional dynamic. Dr Asimakopoulou believes it allows the dental practitioner to demonstrate that they are a caring, empathic, patient-centred healthcare professional. For patients, it could help reframe existing oral health habits and enable them to embed new oral care behaviours both for their partials and their remaining teeth.
Changing oral health regimes can utilise the standard COM-B behaviour change model:
Conclusion
For patients, having to adjust to life after tooth loss and adapting to wearing a partial need not be a negative experience. Improved function, aesthetic benefits and overall improvements in oral health quality of life are highly motivating. For dental practitioners, harnessing this pivotal moment can help them educate and encourage new oral health behaviours, while also strengthening their patient relationships.
As Dr Rawdin says: “I see them a few times a year once all their treatment is done. It's the home care that we're really focusing on to make sure that they're taking good care of everything.”
Expert advice: patient tips for adjustment to partials
Patient Support Leaflet
Download the patient leaflet and equip your patients to stand up to further tooth loss